안녕하세요 닥터부입니다.
오늘은 갑상선수질암에 대해 정리 해보겠습니다!

정의 Definition
갑상선 수질암은 갑상선암의 일종입니다. 갑상선암은 세포의 유형에 따라 여포암과 비여포암으로 나뉩니다.
대부분의 갑상선암은 여포암에 속하는 유두암과 여포암이고, 비여포암에 해당하는 질환이 수질암입니다.
갑상선 수질암은 갑상선암 중에서도 희귀한 암에 속하며, 전체 갑상선암 중 약 0.5~1% 정도를 차지합니다. 수질암은 체내 칼슘양을 조절하는 호르몬 분비 세포에서 발병하는 것으로 알려져 있습니다.
Medullary thyroid cancer is a type of thyroid cancer. Thyroid cancer is divided into follicular cancer and non-follicular cancer according to the type of cell. Most thyroid cancers are papillary and follicular cancers belonging to follicle cancer, and medullary cancer is a disease corresponding to non-follicular cancer.
Medullary thyroid cancer is one of the rarest thyroid cancers and accounts for about 0.5 to 1% of all thyroid cancers. It is known that medullary cancer develops from hormone-secreting cells that control the amount of calcium in the body.

원인 Causation
갑상선 수질암은 갑상선 세포에서 생긴 암이 아니라, 체내 칼슘량을 조절하는 칼시토닌이라는 물질을 만들어내는 C세포에서 발병하는 암입니다. 갑상선 수질암은 RET라는 돌연변이 유전자가 발견되고 이로 인해 기능이 항진되면 발병합니다. 또한 부모에게 RET 유전자를 물려받아 수질암이 발병하는 경우도 있는데, 이는 가족성 갑상선 수질암이라고 합니다.
Medullary thyroid cancer does not originate from thyroid cells, but from C cells that produce a substance called calcitonin that regulates the amount of calcium in the body. Medullary thyroid cancer develops when a mutant gene called RET is found and causes hyperfunction. Also, some cases of medullary cancer are caused by inheriting the RET gene from parents, which is called familial medullary thyroid cancer.
증상 Symptom
갑상선암은 건강검진 때 갑상선의 결절을 발견하면서 우연히 알게 되는 경우가 많습니다. 간혹 목에 결절이 만져지며 그것이 갑자기 커지기도 합니다. 목소리가 변하고 음식을 삼키기 어려운 경우도 있습니다. 하지만 대부분 증상이나 통증이 없습니다.
Thyroid cancer is often discovered incidentally when a thyroid nodule is discovered during a medical examination. Occasionally, a nodule is palpable in the neck, which may suddenly become large. In some cases, the voice changes and it is difficult to swallow food. However, in most cases there are no symptoms or pain.

진단 Diagnosis
① 갑상선 초음파 검사 Thyroid Ultrasound
갑상선 종양의 크기와 위치, 모양 등을 확인할 수 있습니다.
You can check the size, location, and shape of the thyroid tumor.
② 미세침 흡인 검사 Fine needle aspiration test
갑상선암을 진단하기 위한 가장 정확한 검사입니다. 초음파로 갑상선을 관찰하면서 매우 가는 바늘로 갑상선을 직접 찔러 그 세포를 채취하는 검사 방법입니다.
It is the most accurate test for diagnosing thyroid cancer. This is a test method that collects cells by directly piercing the thyroid gland with a very thin needle while observing the thyroid gland with ultrasound.

③ PET/CT
갑상선암이 다른 조직으로 전이되었는지 판단할 때 활용하는 검사 방법입니다.
This test method is used to determine whether thyroid cancer has spread to other tissues.
④ 혈액 속 칼시토닌 양 측정 검사 Calcitonin Blood Test
수질암은 칼시토닌을 분비하는 C세포에서 발생하므로, 칼시토닌 양을 측정하는 것은 이 병을 진단하는 필수적인 검사입니다.
Since medullary cancer occurs in C cells that secrete calcitonin, measuring the amount of calcitonin is an essential test for diagnosing this disease.
치료 Treatment
갑상선 수질암의 근본적인 치료 방법은 수술입니다. 수질암은 다발성인 경우가 많고, 비교적 잘 전이되며, 수술 후에 방사성 요오드 치료가 잘 듣지 않기 때문에 초기에 적극적인 수술이 필요합니다.
수술 후에는 갑상선호르몬제를 복용합니다. 수술 후 암이 재발할 가능성도 있으므로, 정기적으로 검진 및 혈액 검사를 시행하여 재발 여부를 빨리 발견해야 합니다.
The basic treatment for medullary thyroid cancer is surgery. Since medullary cancer is often multiple, metastasizes relatively well, and radioactive iodine treatment does not work well after surgery, aggressive surgery is required at an early stage.
After surgery, thyroid hormones are taken. Since there is a possibility that cancer may recur after surgery, regular checkups and blood tests should be performed to detect recurrence as soon as possible.

경과 Progress
갑상선 수질암은 유두암이나 여포암에 비해서는 예후가 좋지 않은 편입니다. 진단 시 다른 조직으로 전이된 경우가 약 50% 정도이기 때문입니다. 처음 발견될 때 수질암이 갑상선 내에만 있는 경우에는 예후가 훨씬 좋습니다.
Medullary thyroid cancer has a poorer prognosis than papillary or follicular cancer. This is because about 50% of cases of metastasis to other tissues at the time of diagnosis. If the medullary cancer is only within the thyroid gland when it is first detected, the prognosis is much better.
주의사항 Caution
갑상선호르몬제는 아침에 일어나자마자 공복에 복용해야 합니다. 혹은 식사 후 최소 30분의 시간을 두고 복용해야 합니다. 다른 약과 함께 복용하면 흡수에 영향을 줄 수 있으므로 단독 복용해야 합니다. 혈액 검사를 시행하는 날은 먼저 피를 뽑고 약을 복용하면 됩니다. 정기적으로 혈액 검사를 시행하여 혈중 갑상선호르몬 농도를 측정해야 하며, 용량 조절은 반드시 주치의와 상의해야 합니다. 갑상선호르몬제는 평생 복용해도 안전합니다. 임신과도 상관이 없으며, 오히려 임신 중에는 호르몬 조절을 위해 꼭 복용해야 합니다.
Thyroid hormones should be taken on an empty stomach as soon as you wake up in the morning. Or, take it at least 30 minutes after a meal. It should be taken alone as it may affect absorption when taken with other medications. On the day of the blood test, you need to draw blood first and take the medicine. Blood tests should be performed regularly to measure the level of thyroid hormone in the blood, and dosage adjustments should be discussed with the attending physician. Thyroid hormones are safe to take for life. It has nothing to do with pregnancy, but rather, it must be taken during pregnancy to control hormones.

문제
A 25-year-old man presents with the complaint of having a lump in the front of his neck. He says that he first noticed the lump a few weeks ago while taking a shower. Since then, it has not increased in size. He denies any pain or difficulty in swallowing. Past medical history is unremarkable. Family history is significant for his father who had his thyroid removed when he was around his age but doesn’t know why. A review of systems is significant for occasional episodes of anxiety that include a pounding headache, racing heart, and sweating. Temperature is 37.2°C (99.0°F), pulse is 88/min, respirations are 14/min, and blood pressure is 133/87 mm Hg. He is 183 cm (6 ft 2 in) tall with long extremities. There is a palpable 4 cm x 4 cm (1.6 in x 1.6 in) nodule in the left lobe of the thyroid. Which of the following is the most likely pathology in this patient?
| A. Giant cell thyroiditis6% B. Anaplastic carcinoma2% C. Papillary carcinoma21% D. Follicular adenoma18% E. Medullary carcinoma50% |
Explanation:
Correct answer E: Medullary thyroid carcinoma (MTC) is a malignant tumor of the parafollicular cells (C cells) of the thyroid. MTC represents 5-10% of thyroid cancers with a 1-2% incidence in nodular thyroid diseases. It is the third most common malignant tumor of the thyroid, after papillary and follicular carcinoma, which arise from follicular cells. The C cells secrete calcitonin which increases the excretion of calcium to aid in serum calcium homeostasis. The tumor contains amyloid deposits because the large amounts of calcitonin produced by the tumor deposit in the thyroid gland as a type of amyloid. Diagnosis is usually made by fine-needle aspiration biopsy. Approximately 25% of these cases are hereditary due to a germline mutation in the RET proto-oncogene on chromosome 10, which is inherited in an autosomal dominant pattern, forming part of a constellation of two distinct syndromes of endocrine tumors, known as multiple endocrine neoplasia (MEN) type 2A and MEN 2B (see image below). MEN 2B is characterized by medullary carcinoma of the thyroid, pheochromocytoma, "marfanoid" body habitus, and mucosal ganglioneuromas (usually just called "neuromas"). The appearance of the patient in the vignette is described as marfanoid, and he describes a likely family history of medullary carcinoma of the thyroid since his father had a total thyroidectomy at a young age. The periodic episodes of anxiety, with headache, racing heart, and sweating suggest that there is a coexistent pheochromocytoma.
Multiple endocrine neoplasia type 1 (MEN1) is a rare autosomal dominant disorder characterized by a predisposition to tumors of the parathyroid glands, anterior pituitary, and pancreatic islet cells. Other neoplasms can also be seen in this disorder. Most patients have mutations in the MEN1 tumor suppressor gene (protein product: "menin") which is located on chromosome 11.
A popular mnemonic used to remember the associated neoplasias in the MEN syndromes is:
MEN I (3 Ps): Pituitary, Parathyroid, Pancreatic
MEN IIa (2Ps, 1M): Pheochromocytoma, Parathyroid, Medullary Thyroid Ca
MEN IIb (1P, 2Ms): Pheochromocytoma, Medullary Thyroid Cancer, Marfanoid habitus/mucosal neuroma
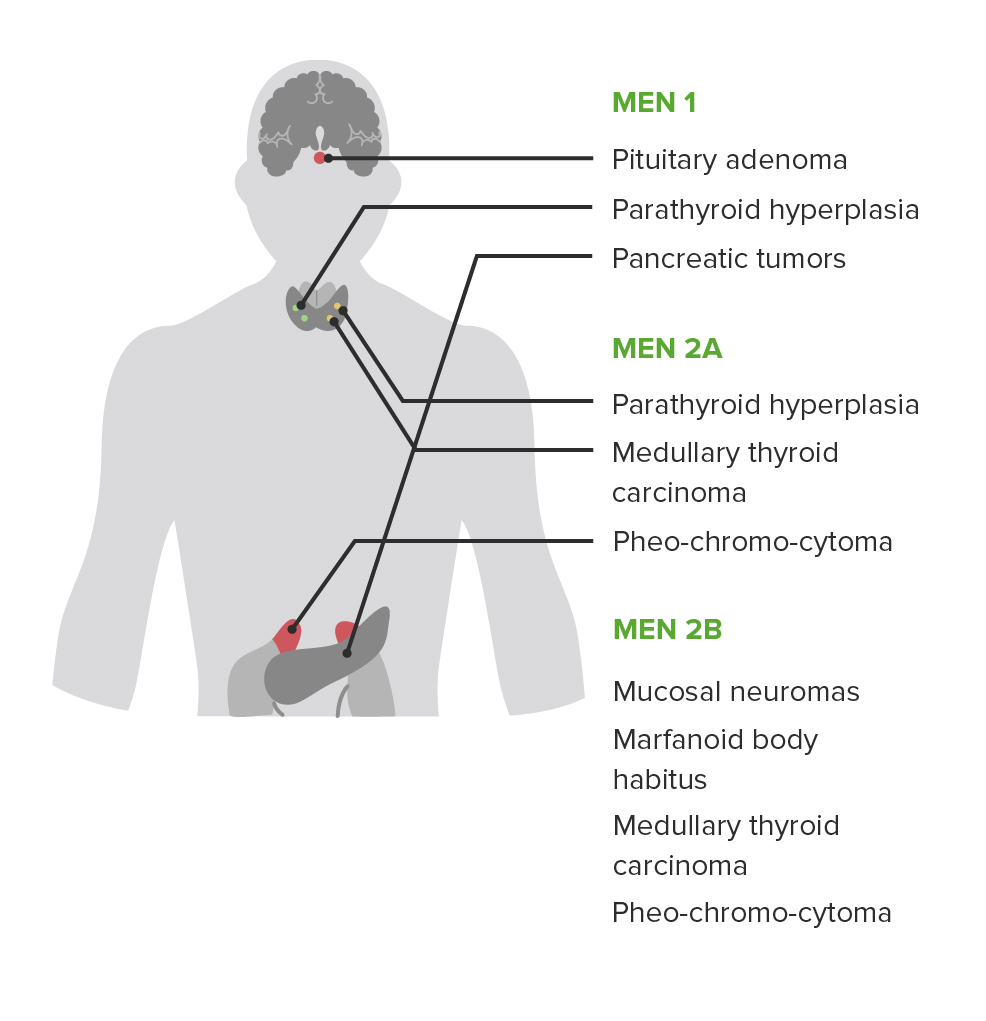
사진 삭제
사진 설명을 입력하세요.
Image: Types of multiple endocrine neoplasias. By Lecturio
Option A: Giant cell thyroiditis, is also known as De Quervain’s thyroiditis or subacute granulomatous thyroiditis. Giant cell thyroiditis is a resolving thyroid syndrome characterized by transient hyperthyroidism or hypothyroidism. Clinically, these patients present with a tender thyroid nodule following a viral upper respiratory infection. Histologically, giant cell thyroiditis is characterized by granulomas. This patient is not exhibiting these symptoms, nor does he have a history of a recent viral infection, making this diagnosis unlikely.
Option B: Anaplastic carcinoma of the thyroid is a malignant tumor of undifferentiated cells. It is most often seen in the elderly and has an aggressive course with a poor prognosis. Most cases are diagnosed due to a local invasion which can present as dysphagia, hoarseness, and difficulty breathing. On physical exam, the thyroid will be non-tender and hard. This is important because anaplastic carcinoma clinically mimics fibrosing thyroiditis–a form of benign fibrosis of the thyroid gland. Anaplastic carcinoma is strongly associated with older patients, making it an unlikely diagnosis in this patient.
Option C: Papillary carcinoma of the thyroid is the most common type of thyroid cancer. Papillary carcinomas are malignant tumors with a characteristic appearance of papillae made of cells with large clear nuclei (known as ‘Orphan Annie eye’ nuclei). Psammoma bodies and nuclear grooves are also typically present. The most common association with the development of this disease is prior exposure of the head and the neck to radiation, especially in childhood. This patient’s presentation does not suggest papillary carcinoma.
Option D: Follicular adenoma is a benign tumor of the thyroid due to the proliferation of thyroid follicles. They typically appear as solitary nodules and are surrounded by a fibrous capsule. Histologically, follicular adenomas cannot be distinguished from follicular carcinoma of the thyroid on a fine needle aspiration. Therefore, resection is the treatment of choice. Follicular adenomas can be ‘hot’- in that, they secrete thyroid hormone, or ‘cold’–in that they are not functional. This patient’s presentation fits more closely with MEN2.
Learning objective: Thyroid nodules have a variety of etiologies, which can be differentiated based on associated symptoms, demographics, and histopathologic findings. Medullary carcinoma of the thyroid is associated with MEN2, which can be identified by the inheritance pattern of the symptoms associated with the other pathologies (e.g., pheochromocytoma and marfanoid body habitus).
| Related Videos: Recurrent Laryngeal Nerve Injury, Anaplastic & Medullary Thyroid Cancer03:54 min 0% Complete Multiple Endocrine Neoplasia Type 2 (MEN Syndrome)01:58 min 0% Complete |
| Book References: First Aid for the USMLE Step 1 (2021, 31st ed): 351, 360 First Aid for the USMLE Step 1 (2020, 30th ed): 351, 343 First Aid for the USMLE Step 1 (2019, 29th ed): 347, 340 First Aid for the USMLE Step 1 (2018, 28th ed): 347 First Aid for the USMLE Step 1 (2017, 27th ed): 339 |
댓글